

At Ari Pediatric Dentistry in London, Ontario, we provide specialty dental treatments for children who require additional care, support, or accommodations. Our pediatric dental team is experienced in treating children with unique medical, developmental, behavioral, or emotional needs in a safe and compassionate environment.
These specialty treatments are designed to help every child receive comfortable, effective dental care regardless of their individual needs.
An infant frenectomy is a procedure used to treat lip ties and tongue ties that may interfere with feeding, comfort, and early development.
A lip or tongue tie occurs when the tissue connecting the lip or tongue is too tight or restrictive, limiting normal movement.
Painful feeding for parent or infant
Decreased milk transfer or production
Gas and/or colic
Loud sucking or clicking noises during feeding
Messy feeding
Difficulty staying latched to breast or bottle
Acid reflux
Poor weight gain or failure to thrive
A frenectomy is a minor same-day surgical procedure used to correct a lip or tongue tie.
In infants, this procedure is typically quick and performed with the goal of improving feeding function and comfort.
If you suspect your child may have a lip or tongue tie, we recommend scheduling a consultation with our specialized pediatric dental team for an assessment.
Comprehensive care from our specialized team includes:
Consultation and assessment with our doula and pediatric dentist
Gentle, thorough explanation of the procedure and aftercare expectations to ensure informed consent
After-hours access to our doula and pediatric dentist for questions or concerns
In-person or virtual follow-up visits to assess healing and provide continued support
Optional additional feeding support with our doula, upon request
Sedation options available for toddlers and children when appropriate
We use LightScalpel CO₂ laser technology for frenectomy procedures when clinically appropriate. LightScalpel C02 Laser Frenectomy:
Minimized bleeding, reduced swelling and discomfort
Lower risk of infection
Shorter procedure time
Smoother healing and recovery
At Ari Pediatric Dentistry in London, Ontario, we provide special care dentistry for children who require additional support, accommodations, or individualized treatment approaches due to medical, developmental, behavioral, or emotional needs.
Special care dentistry focuses on improving the oral health of children who have physical, sensory, intellectual, developmental, medical, or emotional conditions that may make traditional dental care more challenging.
Oral health is an important part of a child’s overall health and daily life. Children with cognitive or developmental disabilities may be at higher risk for dental cavities and gum disease, which can affect comfort, nutrition, and daily activities.
Special Care Dentistry benefits patients by taking a comprehensive view of oral health, and working with all members of an individual’s care team to achieve the most appropriate and integrated care plan and treatment. Our pediatric dental team works closely with families and other healthcare providers when needed.
If you have questions about special care dentistry or would like to discuss your child’s specific needs, we recommend contacting our office to schedule a consultation.
Protect your child’s future smile
Save time and money by addressing concerns early
Fewer dental appointments over time
Boost your child’s confidence
Support proper speech and eating development
Could your child need early orthodontic treatment? The Canadian Association of Orthodontists says that the perfect time for an evaluation is between 6 and 8. Our pediatric dentists in London, Ontario use this evaluation to monitor growth and plan future care if needed. This is when the first permanent molars emerged, making it possible for any of our London pediatric dentists to notice any emerging concerns. While treatment may not be necessary until years down the road, this appointment will give you an idea of what to expect and have a plan in place for the future.
Did you know… your child can inherit orthodontic issues or they can be the result of dental disease, abnormal swallowing, or injury.
Speech difficulties
Crooked or misaligned teeth
Difficulty chewing or biting food
Upper or lower jaws that appear too large or too small
Crowding as permanent teeth come in
Biting the lips or cheeks while chewing
While your child still has baby teeth in their mouth, there are various problems we can detect including crossbites, underbites, excessively spaced teeth, teeth that meet abnormally or not at all, crowding, and problematic thumb sucking that is detrimental to the development of the teeth and jaws.
At Ari Pediatric Dentistry, we see children from infancy through their teenage years. We have several programs and services that can make a difference in the development of your child’s smile. We know that it can be easier to treat certain orthodontic conditions earlier rather than later. So, don’t hesitate to reach out and speak to our team!
Improved overall body function and development
Supports maximum growth potential
Increased energy and focus
Helps children reach their full developmental potential
Encourages healthier breathing habits
Airway-focused dentistry evaluates how breathing patterns, oral posture, and jaw development affect a child’s overall health.
There are many reasons why you should breathe in through your nose instead of the mouth. You’re able to take deeper breaths, which provides more oxygen to the body. And that makes for healthy tissue and organ function. Other wonderful benefits include balanced pH levels, a feeling of calmness, and better athletic performance. Proper breathing through the nose is essential. At Ari Pediatric Dentistry, we realize this, and it’s why we offer airway-focused dentistry.
According to research published by the National Library of Medicine, approximately half of all children regularly breath through their mouths. Unfortunately, most parents and kids are unaware of how this could be harming their health and development. Early identification allows pediatric dentists to guide growth and reduce potential long-term concerns.
Sleep-disordered breathing, including obstructive sleep apnea
Crowded or misaligned teeth
Frequent infections (such as tonsils or ears)
Bedwetting
Low energy levels
Picky eating
Altered facial growth patterns
During a pediatric dental evaluation, we assess whether mouth breathing may be affecting your child’s oral and facial development and discuss appropriate next steps. Depending on our findings, we may recommend monitoring, myofunctional therapy, or a frenectomy when clinically appropriate.
If you have concerns about your child’s breathing or development, we recommend scheduling a consultation with our pediatric dental team.
easier breathing
reduce headaches
a better night’s sleep
minimize the risk of gum disease
better digestion
If your child is having difficulty breastfeeding, chewing, swallowing, or speaking, they may need to undergo myofunctional therapy – available at Ari Pediatric Dentistry.
Orofacial myofunctional therapy retrains the orofacial muscles and helps correct a range of functional disorders, including:
mouth breathing
improper chewing
unusual swallowing
poor tongue rest position
Orofacial Myofunctional Disorders (OMD) often go unrecognized in children and adults and can affect breathing, swallow patterns, muscle tension, and the ability to chew foods properly. OMDs are a symptom of functional and structural changes that lead to abnormal growth and development of the facial structures. TMJ issues, grinding, clenching, nail-biting, sleep breathing disorders, tooth pain, headaches, and neck pain are all possible symptoms of a myofunctional disorder or tongue tie.
At Ari Pediatric Dentistry, our goal is to educate and create awareness of orofacial myofunctional therapy and help in the individual development and reeducation of orofacial muscles to correct swallow patterns and improve airways in children.
At proper rest, the tongue should naturally rest on the mouth’s roof inside the upper teeth. The lips should be sealed. This proper rest position helps in the development of the upper palate and facial bones.
A good swallow pattern allows the tongue to create a proper seal while swallowing. The front of the tongue should be resting on the palate while the back of the tongue carries the food to the back of the mouth.
The main goals of therapy are to achieve a proper swallow pattern and proper rest position of the orofacial muscles. This includes promoting a lip seal, preventing parafunctional habits, promoting correct chewing patterns, and developing airway and promoting nasal breathing. This involves simple exercises done two to three times per day.
This stage of therapy is ongoing for several weeks but can be done independently. There will be periodic check-ins with the myofunctional therapist to change the exercises according to the needs of the individual.
Orofacial myofunctional therapy may improve some of the following:
swallow patterns
muscle tension in head and neck
headache relief
airway and breathing
digestion
dental arch development-correct chewing patterns
lower risk of periodontal disease
improve facial tissue tone
facial development
quality of sleep
speech (if speech is the primary concern, a referral will be made to a speech and language pathologist)
Myofunctional therapy needs commitment from clients and parents to achieve the maximum benefits of proper swallow patterns and orofacial rest positions.
This appointment takes about 60-90 minutes. Oral function, occlusion, and extensive medical and psycho/social history will be collected. Diagnostic photos will be taken and a detailed treatment plan created. An orofacial myofunctional therapist will do this, but a dentist will complete the tongue assessment and diagnosis.
These appointments are 30-45 minutes and involve assessing 0rofacial function, motivational interviewing, education, and implementation of Myofunctional therapy exercises where indicated. The exercises are simple and should take no longer than 10 minutes, two to three times per day. The sessions can be in person or virtually. These myofunctional therapy appointments are scheduled according to your child’s needs.
Often the therapy is done in association with a tongue tie and/or lip tie release. Before this procedure, some exercises may be required to strengthen the head, neck, and tongue muscles to allow better function post-operatively.
After the tongue is released, there will be additional myofunctional therapy sessions. The goals of therapy are different for each person. They include:
palatal tongue placement during swallowing, speech & at rest
correct swallowing
good nasal breathing both day and night
The number of myofunctional therapy sessions varies from person to person. Therapy is complete once good oral function has become habitual.
Have any questions about myofunctional therapy? Contact our team at your London pediatric dentist today!
During development, the tongue starts off completely attached to the floor of the mouth. Once the tongue is fully formed in utero around week 8, it begins to separate from the base of the mouth, becoming free to move around.
The lingual frenulum is the name given to the connective tissue remnant under the tongue that serves to support and limit its movement in different directions. Yes, every person is born with one!
For approximately 5-10% of babies, the tongue and floor of mouth separation process is disrupted in utero, leading to an abnormally short frenulum. The presentation can vary widely in thickness, elasticity and specific location on the tongue and floor of the mouth. Sometimes a frenulum may completely tether the tip of the tongue to the edge of the lower jaw. Different presentations may restrict tongue range of motion to varying degrees, and may impact oral motor development, feeding skills and breathing habits even in infancy.
The medical term for tongue tie is “ankyloglossia” and studies show the defect is hereditary. A tongue tie diagnosis and treatment recommendation should be made based upon a true functional limitation. Simply seeing a frenulum under the tongue does not mean it is restricting tongue range of motion. Feeding assessments from appropriate specialists provide crucial insights on a baby’s oral motor skills and it takes an experienced provider to thoroughly investigate anatomical presentation and associated symptoms.

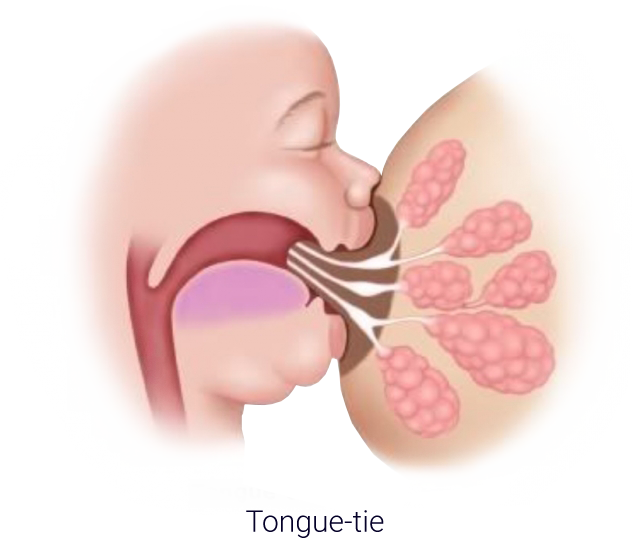
During infancy, the tongue needs full range of motion to create adequate suction to express milk from the breast. The front-mid portion of the tongue draws in, cups and compresses breast tissue while strength and flexibility in the mid-back portion of the tongue is needed to create the negative pressure to remove milk from the breast.
A baby with a tongue tie may be unable to latch deeply onto the breast, leading to possible nipple pain and damage. When the tongue cannot extend up and over the lower jaw, a baby’s latch may feel uncomfortable. Maintaining a latch could pose as a challenge for these babies; some may remain attached to the breast for long periods of time without taking in enough milk.
When the suction is compromised and a baby repetitively loses the seal at the breast or bottle, milk can consistently spill out the sides of the mouth and air may be swallowed, leading to excess gas and fussiness. A tongue tie may impact oral motor coordination and feeding efficiency at the breast or bottle.
Just like under the tongue, every baby is born with connective tissue under the upper lip, called the labial frenulum. This tissue helps to anchor the lip to the jaw for proper movement and facial development. Almost 90% of babies are born with a frenulum that attaches to the lower edge of the gum line – the presence of the tissue is normal anatomy. As children get older and the jaw develops, the labial frenulum attachment has been shown to shift upward.
An abnormally tight labial frenulum can disrupt the seal around the breast or bottle nipple, leading to increased air intake – contributing to reflux and gas symptoms or breast pain from the tight upper lip. The lip should play a passive role when a baby is feeding, gently rounding to maintain the seal at the breast or bottle nipple so milk doesn’t spill out. In toddlerhood, a short labial frenulum may impact a child’s comfort forming a seal on a straw or clearing food from a spoon.
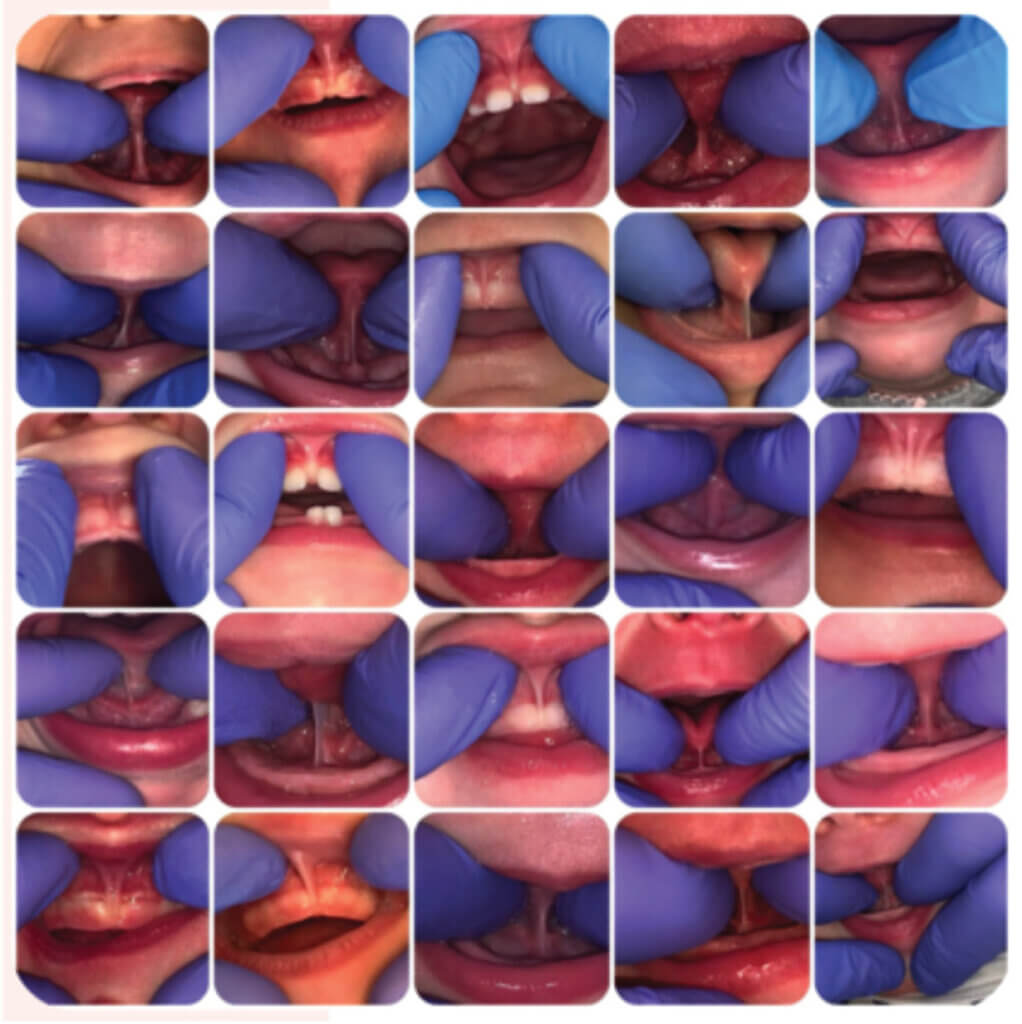
This photo gallery illustrates a variety of anatomical presentations of lingual and labial frenula. Some of these babies were diagnosed with tongue or lip ties while others presented with functional, flexible connective tissue allowing for full range of motion. It takes an experienced provider to investigate anatomical presentation (taking into account the variations in clinical appearance), tongue function and associated symptoms.
In order to direct airflow in and out of the nose, the tongue must be able to rest up against the roof of the mouth. When we breathe through our nose, we can efficiently humidify and filter the air and improve oxygen circulation in our bodies! A tongue tie physically pulls the tongue down towards the floor of the mouth, making it challenging and sometimes impossible to achieve a tongue to palate seal. Low tongue posture may lead to snoring and disrupted sleep patterns.
At rest, the consistent pressure of the tongue against the palate, balanced by the pressure provided by proper lip sealing, serves as a guide for the growth of our upper jaw. Literature shows children with untreated tongue ties may develop abnormal tongue function early in life with a secondary impact on orofacial growth and sleep disordered breathing
While the following symptoms are common amongst babies and their mothers, it is important to note that these signs can be linked to other factors and feeding challenges – they are not solely related to ties.
Babies/toddlers may exhibit:
Mothers may experience:
Prior to having a tongue or lip tie evaluation, children should be assessed by an International Board Certified Lactation Consultant (IBCLC) or feeding specialist (a trained SLP or OT).
Lactation consultants are experts in guiding mothers throughout their feeding journeys and addressing concerns regarding milk supply, latch comfort, breast and bottle feeding techniques, infant feeding patterns, positioning and so much more.
Some speech language pathologists or occupational therapists have special training to become experts in pediatric feeding and swallowing; they can assess and address concerns regarding oral tone, strength and oral motor coordination in infancy and childhood.
Working with a functional specialist provides important insight on oral reflexes, postural habits, or speech (if age appropriate) to help differentially diagnose the root cause of the child’s symptoms or to clarify a potential link between a short frenulum and the symptom presentation.
A tongue or lip tie release (called a frenectomy) is a minor surgical procedure that removes the tight frenulum, allowing for improved range of motion and flexibility. Because the frenectomy addresses an anatomical limitation, it aids in shifting the physiology in order to reduce or eliminate symptoms.
Many children are able to quickly adapt and thrive following the procedure. Others may take some time to adjust to the new movement and benefit from continued support from an oral motor/feeding specialist to optimize their oral strength and skills. Consideration of other therapeutic modalities may be helpful.
A pediatric craniosacral therapist, osteopath or chiropractor can help babies to release tight fascia/muscles that have compensated for a short frenulum or improper suck. Such therapy aims to calm the nervous system and improve structural mobility to assist with latch, feeding, sleep, movement, mood and digestion.
A physical therapist or occupational therapist can address range of motion limitations, weak or tense body tone, sensory motor difficulties, and asymmetries in physical development.
Some children may benefit from working with an oral motor or bodywork specialist in preparation for or following the frenectomy procedure. Each case needs to be assessed by a trained practitioner on an individual basis.
Book a visit to DentiCare, simply fill out the form below and we will contact you back regarding the intervention you require.
Children may benefit from myofunctional therapy if they experience mouth breathing, difficulty chewing or swallowing, speech issues, poor tongue posture, sleep-related concerns, or persistent oral habits. A pediatric dental evaluation can help determine if therapy is appropriate.
Myofunctional therapy may help address mouth breathing, improper swallowing patterns, poor tongue rest posture, abnormal chewing habits, and airway-related concerns. It is also commonly used alongside orthodontic treatment or airway-focused care.
The lingual frenulum is a band of connective tissue located under the tongue. Everyone is born with a lingual frenulum, and its function is to support and limit tongue movement in different directions.
A tongue tie, medically known as ankyloglossia, occurs when the lingual frenulum is unusually short, thick, or restrictive, limiting normal tongue movement. Tongue ties vary in appearance and severity and are diagnosed based on functional limitations rather than appearance alone.
Tongue ties affect approximately 5–10% of infants. Not all tongue ties require treatment, and recommendations are based on how tongue movement impacts feeding, breathing, or oral development.
A tongue tie may interfere with a baby’s ability to latch, maintain suction, and transfer milk effectively. This can contribute to feeding difficulties, prolonged feeding times, clicking sounds, reflux symptoms, or poor weight gain in some infants.
No. Treatment is recommended only when a tongue tie causes functional limitations. A thorough assessment by experienced providers is important to determine whether intervention is necessary.
Yes. Myofunctional therapy is often recommended before or after tongue tie treatment to support proper muscle function, swallowing patterns, and long-term oral development.
The best way to determine whether myofunctional therapy, tongue tie treatment, or monitoring is appropriate is to schedule a consultation with a pediatric dental team experienced in airway-focused and functional care.

As a pediatric dentist in London at Ari Pediatric Dentistry, we love looking after the oral health of children of all ages in our community. Contact us today! We’ll help your child get started on the right foot.